Natalia Trayanova, the biophysicist who creates virtual hearts: ‘We are facing the largest known killer’
The researcher designs digital twins for every patient that help facilitate surgeries for serious cardiac problems


A healthy heart beats approximately three billion times throughout its lifetime. This happens thanks to a small ‘brain’ of 40,000 neurons and other nerve cells that generate electric pulses that contract the heart in order to pump blood to the rest of the body. When this system fails, the heartbeat becomes irregular, which can cause a cardiac arrest in a matter of minutes, or trigger other health conditions, like a stroke, over the years.
Natalia Trayanova faces the “enormous” public health concerns associated with cardiac failure every day. A Bulgarian biophysicist, she is a professor of biomedical engineering and medicine at Johns Hopkins University, where she directs the Alliance for Cardiovascular Diagnostic and Treatment Innovation, a research institute where doctors, engineers, radiologists and mathematicians apply techniques based on data, computational modeling and innovations in cardiac imaging to improve the diagnosis and treatment of cardiovascular diseases.
Trayanova creates virtual hearts for every patient, an innovation that can improve clinical decision-making and medical care. On a visit to Spain for an event at the Ramón Areces Foundation in Madrid, the scientist explains in an interview that one of the most brilliant uses of artificial intelligence is the simulation of a heart to prevent it from failing ahead of its time.
Question. How dangerous is the disease you’re facing?
Answer. Sudden cardiac arrest is the largest killer we know. In the majority of cases, it’s due to alterations in the cardiac rhythm, arrhythmias. Every year, some 400,000 people die of these causes in the United States alone. It’s an enormous problem, above all because we don’t understand exactly why and how it happens. Our ultimate goal is to know who will suffer an arrhythmia and being able to avoid it.
Q. How do you hope to achieve that?
A. With computational cardiology. Imagine that you come to a hospital with a cardiac problem. In many cases, doctors aren’t clear on the best way to treat it. What we do is create a virtual twin of your heart that helps us to understand what problem you are suffering from and try out treatment options so that doctors can decide what to do.
Q. How does one build a digital twin of the heart?
A. We use medical images and computation to build an exact replica of your heart. It reproduces everything that happens in the organ, from the cellular level to that of the entire heart.
Q. Can you make a twin for any heart?
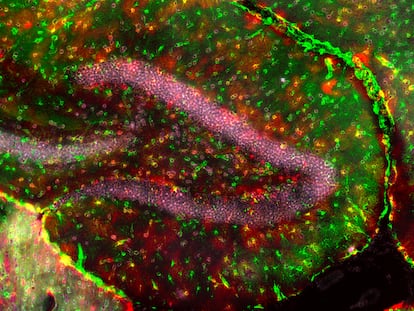
A. The heart has scars that form if you have a stroke. There is also connective tissue that forms from normal aging of the heart. These lesions make it difficult for electrical impulses to propagate, which means that your heart does not contract properly and it doesn’t pump enough blood and oxygen to the rest of your body. In five minutes, you can be dead. The virtual twin is based on an image of the patient’s heart made with contrast-enhanced magnetic resonance imaging. There we can see the scars and reproduce them in a three-dimensional model. In this model, we also include the orientation of the muscle fibers, which are fundamental for contraction. And finally, we add a layer that shows us the heart at the resolution level of one micron [1/25,000th of an inch]. In this layer, we can now represent the tissue at the cellular and subcellular level. We can reproduce, for example, the small electrical currents that pass from one cell to another, which are essential for the heartbeat to spread throughout the heart. A finished virtual heart ends up representing some 20 million cells.
Q. How long does it take to build a virtual heart?
A. It’s a complex process and requires large computers. First, based on an MRI scan, the tissue and fibrosis are segmented, which would take six hours if done manually. However, with artificial intelligence, this process is reduced to a few minutes. Then, software assigns the orientation of the fibers based on an atlas of human hearts. Subsequently, it is divided into small areas before the simulation. The simulation is difficult, due to the high resolution and complexity of the current flow equations, which require very short time intervals to accurately model electrical propaganda. So, to answer your question, simulating an arrhythmia for four minutes can take between four and 10 hours on a supercomputer, depending on the number of CPUS [central processing units] available. However, to do multiple simulations and analyze different scenarios requires a great deal of computational effort. We can evaluate disturbances in different area of the heart and determine the critical points where ablation is necessary, meaning burning tissue to make a small scar to correct an arrhythmia. We recently published a study in Nature Computational Science where we used artificial intelligence to solve the necessary equations in one second. It still needs to be adapted to include scarring and fibrosis, but it is already efficient in a normal heart.
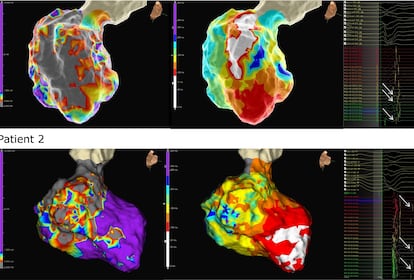
Q. What results have you gotten in patients?
A. Arrhythmias vary according to their location in the heart. Those that affect the lower chambers, the ventricles, cause early death. Those that affect the upper chambers, the atria, aren’t lethal, but they represent the largest problem in global health: 2% of the population suffers from them, one in every four people over the age of 65. These arrhythmias lead to strokes. To treat them, we have developed personalized digital twins for 10 patients in a pilot study. These people have suffered very serious strokes, and their doctors were not sure how to proceed. The digital twins indicated where to perform the ablation and what the results would be. The doctors only had to place the catheter where we told them. We finished three weeks ago and so far, all the patients are alive and in good health. We have also launched a new trial with 170 patients with atrial problems.
Q. Will they be able to use these techniques on a routine basis some day?
A. Right now, their use is limited due to their large computational requirements. But with the new artificial intelligence tools that have been recently released, the equations can be solved in seconds on a personal computer. This will facilitate their implementation in clinics. Currently, the process is automated: the patient arrives, their heart is scanned, it is segmented, the digital twin is created and the ideal treatment is predicted. The night before, the doctor receives the plan and, during the procedure, follows the on-screen prediction to apply the catheter with precision.
Q. What do you think about current misgivings about artificial intelligence?
A. At Johns Hopkins, I direct research in digital twins and computational cardiology as well as the AI initiative in health and medicine. Thanks to an anonymous donor, a large project has been funded that includes 160 AI professors and a new building. Although AI is advancing rapidly, its adoption in medicine is slow due to the need for rigorous testing and doctor trust. It is not enough for AI to make a diagnosis; it must be explainable and understandable to doctors and patients. Building this trust is key to integrating it into clinical practice and medical records.
Q. How is Donald Trump’s new administration impacting your country’s biomedical research?
A. It’s terrible. The cuts to the National Institutes of Health’s indirect costs under the Trump administration are very damaging for research in the United States. These costs, which are negotiated with each university, finance laboratories and infrastructures. Johns Hopkins is the institution that receives the most NIH funding in the entire United States. The new situation will seriously affect scientific development. The reduction in resources will limit the hiring of new professors and hinder the progress of research. The United States risks losing its global leadership in science in biomedicine. It may take several generations to mitigate the impact.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.